Decoding the Gentle Birth Practice
Have you ever heard of umbilical non-severance, also known as lotus birth? In recent years, more families have shown interest in this gentle birth practice, seeing it as part of a larger return to alternative birth practices and cultural birth rituals that emphasize slowness, spirituality, and respect for the birthing process.
In simple terms, a lotus birth means leaving the baby’s umbilical cord and placenta attached until they separate naturally. Instead of cutting the cord, parents wait for natural detachment, which may take several days.
This article will walk you through the lotus birth safety benefits risks, drawing on both evidence and parent experiences. We’ll explore the spiritual and holistic perspectives, the medical contraindications and infection risk placenta, as well as practical tips for caring for the placenta if you choose this path.
It’s worth noting that lotus birth is very different from placenta encapsulation, where the placenta is processed into supplements, or lotus birth vs. delayed cord clamping, which only delays cord cutting for a few minutes to allow for optimal blood transfer. Lotus birth extends this connection for days.
The Philosophy and Perceived Benefits of Umbilical Non-Severance
Gentle Transition and Full Blood Transfer
Supporters of lotus birth often describe it as a way to ease the spiritual transition baby into the world. By allowing gentle cord separation, the process is thought to reduce reduced trauma for baby, giving them time to adjust to life outside the womb.
From a physiological perspective, advocates believe that keeping the placenta attached ensures a full blood transfer placenta, which supports stronger iron stores newborn and healthier early development.
Parents also emphasize natural detachment—waiting for the cord to fall off on its own—as part of a holistic postpartum journey. For many, it aligns with respectful parenting, where the baby’s body is left to make its own choices about separation.
Spiritual and Emotional Connections
On a deeper level, families often describe a profound sense of bonding with placenta. Some see it as the baby’s first companion, or a placenta as spirit companion, symbolizing protection during the delicate early days.
Within the natural parenting community, lotus birth is sometimes referred to as honoring placenta wisdom. While the medical field may regard the placenta as a placenta as biohazard, many parents view it as sacred, deserving rituals such as placenta burial or other placenta rituals.
By extending the fourth stage of birth (extended), lotus birth reinforces the idea that the birth process doesn’t end with delivery, but continues as mother, baby, and placenta remain connected.
Critical Safety and Medical Concerns (The Risks)
The Primary Risk: Infection and Sepsis
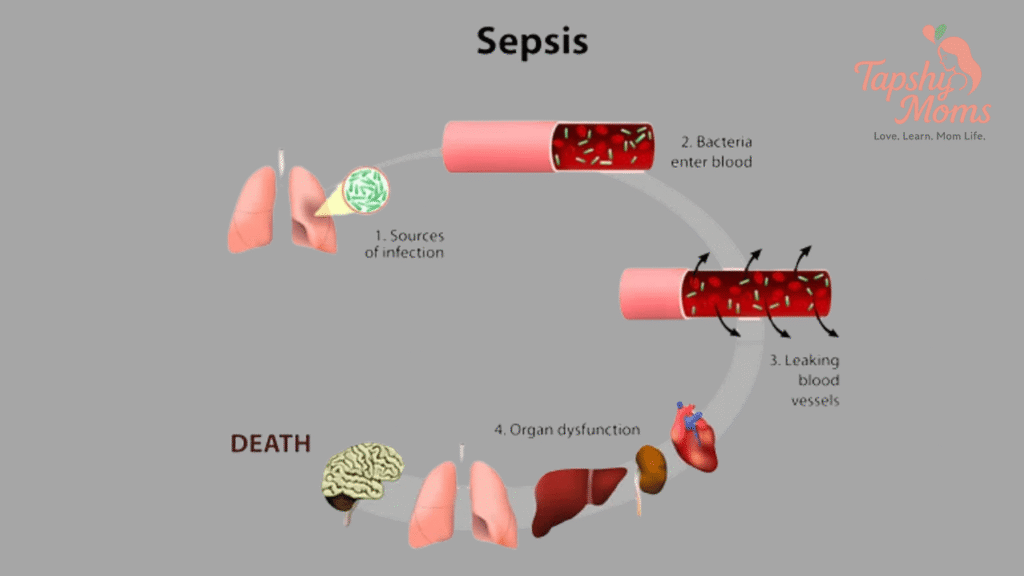
The most pressing concern about lotus birth is bacterial growth placenta. Once the placenta is delivered, it begins to undergo placenta decomposition, no longer receiving oxygenated blood. This creates an ideal environment for bacteria.
The infection risk placenta comes from the possibility that bacteria could travel from the decaying tissue up through the cord, leading to a sepsis risk newborn. Documented cases, though rare, highlight this as a serious danger.
Some parents try to limit risks through hygienic handling placenta, using methods like salt and herb placenta to help with drying and preservation. But these measures do not fully remove the underlying biological risk.
Medical contraindications are especially important: lotus birth should be avoided if there are concerns such as maternal infections (like chorioamnionitis) or complications at delivery.
Medical and Hospital Policy Stance
So, what do doctors say about lotus birth? Most major pediatric and obstetric bodies do not recommend it due to insufficient evidence of benefits and clear risks. Pediatrician advice lotus birth often emphasizes that delayed cord clamping provides proven benefits without prolonged risk.
Hospitals also face logistical issues. Hospital policy lotus birth generally prohibits parents from leaving with the placenta still attached due to placenta transport restrictions and its classification as a biohazard.
Unsurprisingly, this has fueled strong criticisms of lotus birth from medical professionals, who consider the dangers of lotus birth greater than the potential gains.
Process, Practicality, and Care for the Placenta
Practical Placenta Care
If you are considering lotus birth, it’s important to know how to care for lotus birth properly. Here are the essentials:
- Placenta bag or wrap: Use breathable fabrics or specially designed placenta bags to allow airflow.
- Drying the placenta: Apply natural drying agents such as sea salt and aromatic herbs (salt and herb placenta) to reduce moisture and help with odor.
- Umbilical cord care: Keep the cord dry, avoid tugging, and gently reposition the placenta during diaper changes.
- Placenta smell: A mild odor may appear after a couple of days; strong odors can signal improper drying or potential lotus birth complications.
Logistics and Support
Parents often ask, how long does lotus birth take? The typical cord detachment time ranges between 3 and 10 days. During this period, gentle handling is crucial.
Midwife support lotus birth can be invaluable, especially for families planning a home birth lotus birth or even an unassisted birth. A knowledgeable midwife can guide safe practices and help recognize any early signs of complications.
While many families report smooth experiences, lotus birth complications such as premature cord separation, excessive odor, or challenges in caring for the placenta can occur.
Conclusion: Weighing the Evidence and Making a Choice
Lotus birth is a practice steeped in meaning, blending spiritual reverence with a vision of holistic postpartum care. The perceived benefits—such as a spiritual transition baby, deeper bonding, and symbolic respect—can feel deeply fulfilling for some families.
Yet, we cannot ignore the infection risk placenta and the very real dangers of lotus birth. The scientific evidence is limited, and what is known points to a higher risk of complications without proven medical benefit.
The best path forward is an evidence-based birth approach: talk openly with your care provider, weigh your values against the potential risks, and seek pediatrician advice lotus birth before making a decision.
If you’ve walked this path, sharing your parent experiences lotus birth can help other mothers make informed, compassionate choices.
FAQ: Your Questions on Lotus Birth Answered
Is lotus birth safer than delayed cord clamping?
When comparing lotus birth vs. delayed cord clamping, delayed clamping has strong scientific support, offering iron and blood volume benefits without extended infection risks. Lotus birth does not currently have the same evidence base.
What is the minimum cord detachment time and maximum care required for the placenta?
On average, how long does lotus birth take is 3–10 days. Daily drying and careful cord monitoring are required throughout.
Are there any specific medical contraindications for choosing a lotus birth?
Yes. Medical contraindications include maternal or newborn infections, difficult births, or compromised immune systems. Always discuss your specific case with your doctor.
How do you prevent the strong placenta smell during a lotus birth?
Using salt, herbs, and breathable fabrics can help manage placenta smell, but some odor is natural as the placenta dries. Strong or foul odor should be treated as a red flag.
What is the official pediatrician advice on lotus birth in the US and UK?
In both countries, what do doctors say about lotus birth? is largely consistent: pediatricians do not recommend it due to safety concerns, though they support delayed cord clamping.
What are the primary dangers of lotus birth that parents should be aware of?
The main dangers of lotus birth include infection, sepsis, and logistical difficulties in caring for decomposing tissue attached to a newborn.